TMO implants
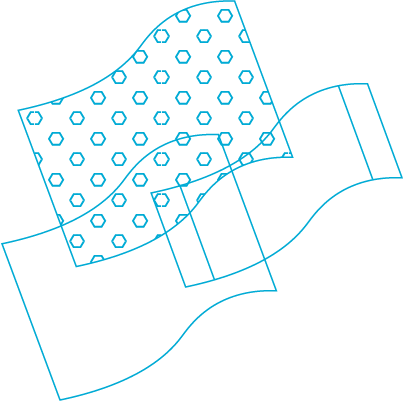
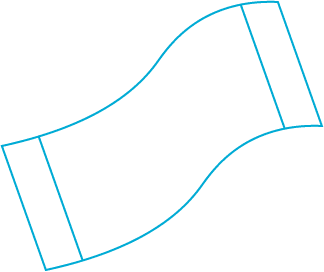
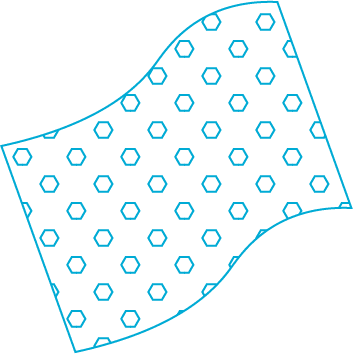
The dura mater substitute implant is a solution for the natural dura mater replacement. The unique design and manufacturing process ensures the implant with better performance and greater tear resistance than other duralumin graft lining materials.
ICONLAB
Нижний Новгород, Россия
Characteristics
The invention relates to medicine, namely to neurosurgery. Under fulfilling surgical operative interventions on the brain for injuries or brain tumors, it often becomes necessary to perform dural plasty (dura mater), which is opened up during surgery.Firstly, it is done with the aim of subdural space seal, secondly, for cicatricial adhesive process prevention with meningeal scar formation in the surgical approach field. Structural- morphological dura mater features and dura mater rigidity don’t allow in some cases under the surgical wound suturing to suture own dura mater by tightening the edges. Thus, the necessity to close the formed dura mater defect by a peculiar “patch” often arises. Autoplasts (aponeurosis, fascia lata), allograft (preserved cadaveric dura mater) and artificial implants are applied as a «patch» There are known resorbable implants for plastic defects of the dura, described in US Pat 6679919, EP 1029553, and non-absorbable implant for plastic dura defects, described in US Pat 5634944 (prototype). These structures are used in neurosurgery as a temporary (in the case of an absorbable implant) or permanent (in the case of a non-absorbable implant) substitute for the dura mater and plastics of dura mater defects.
However, these materials, allowing to solve the problem of subdural space sealing, further undergo biological degradation and do not prevent the development of the cicatricial adhesive process, which ultimately leads to a rather rough scar formation in the area of an operative access.
Firstly, a meningeal scar is a potential epileptogenic focus, secondly, it disrupts the CSF circulation in this area. Undoubtedly, this disadvantage worsens the patient ‘s quality of life in the late postoperative period.